Pressure Ulcer
What is a Pressure UlcerBedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone. People most at risk of bedsores have medical conditions that limit their ability to change positions or cause them to spend most of their time in a bed or chair. Bedsores can develop over hours or days. Most sores heal with treatment, but some never heal completely. You can take steps to help prevent bedsores and help them heal. Prevalence: 4-8% of those that receive healthcare in New Zealand experience a pressure injury1 Incidence: 55,000 people receive a PI annually in the New Zealand health sector |

|
CausesA pressure ulcer is caused by a lack of blood flow due to mechanical stress on the skin and tissues over a bony area that has been under pressure for a prolonged period. If the blood supply is cut off to an area of skin for more than 2–3 hours, the skin is deprived of oxygen and begins to die. Four primary contributing factors for bedsores are:
|
|
|
|
SymptomsWarning signs of bedsores or pressure ulcers are:
|
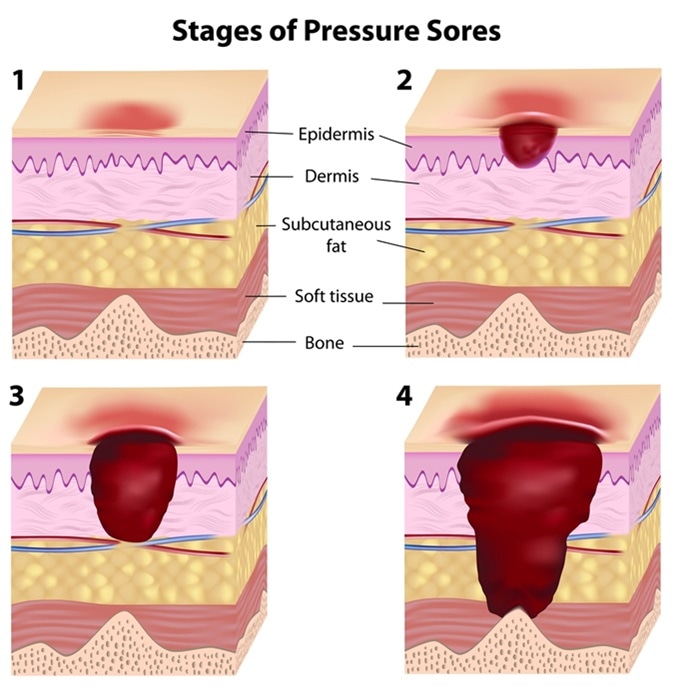
StagesBedsores fall into one of several stages based on their depth, severity and other characteristics. The degree of skin and tissue damage ranges from changes in skin color to a deep injury involving muscle and bone. Pressure ulcers are classified into stages according to wound severity. Stage 1
Stage 2
Stage 3
Stage 4
|
|
What is the treatment for a pressure ulcer?Evidence suggests that up to 95% of PI are avoidable when appropriate interventions are in place. A pressure ulcer can be difficult to treat once it has gone beyond stage 2. In the early stages when the skin is still intact, a pressure ulcer usually heals by itself if the pressure has been removed. Once the skin is broken, the main aim is to prevent infection and protect the sore so that it can heal. Dead tissue may be removed with a scalpel (debridement). Deep pressure ulcers are very difficult to treat and often require surgical treatment to remove dead and decaying tissue.
|
Prevention
|
|
Our solutionsLevabo Heel up® and All up® - Single-patient inflatable positioning cushions.Heel up® and All up® is suitable for effective prevention and treatment of pressure ulcers in high-risk areas such as heels, hips, elbows, shoulders, back, etc Levabo Turn AllAutomated anti decubitus lateral turning system for pressure ulcer prevention. Automatic side positioning system 0-30 degrees for pressure ulcer prevention or treatment TrulifeThe Trulife range of pressure relieving positioning devices were developed as a result of their commitment to provide improved levels of pressure care for patients and undergoing Theatre procedures.
Protect-A-LimbProtects the limbs from skin tears and skin damage. It is light in weight and yet bulky enough to protect. |